Held to Ransom: What happens when investment firms take over UK care homes
Christine Corlet Walker, Vivek Kotecha, Angela Druckman and Tim Jackson
CUSP Working Paper Series | No 35

Summary
The involvement of investment firms in the UK’s adult social care sector is a cause of mounting concern. Many of the strategies that investment firms use to achieve returns for their investors expose whole chains of care homes to large costs and increase the risk of bankruptcy and closure. This ‘financialisation’ of care has been implicated in the high-profile collapse of several large care home chains. However, little research has been done looking at the direct impact of these strategies on workers and service users in the care homes themselves.
In this report, we present the findings from a series of interviews with care workers who were working in care homes during, or shortly after, they had been taken over by an investment firm. Our respondents expressed five key concerns about the behaviour of their new employers. Specifically, they felt that their care companies were:
- exploiting care staff;
- cutting corners on service delivery;
- covering up mismanagement;
- failing to communicate; and
- prioritising profit over care.
We also studied the financial accounts of fifteen of the largest care home chains in the UK and uncovered a large and widening disparity between the pay of directors and the wages of employees. This pay gap was growing particularly fast in investment-firm-owned chains. The pay ratios between the highest paid director and the average employee within the care companies in our sample were similar to those ratios found in large for-profit companies in other sectors, but far higher than those found in public services like the UK’s National Health Service. This disparity existed even for some not-for-profit groups.
Our analysis paints a picture of a sector that is deeply unfair, not only in terms of who benefits from the financialisation of care, but also in terms of who pays the price. We contend that achieving a care sector that works for workers and service users rather than investors and profiteers means removing the profit motive altogether, reducing the size and complexity of care home groups, and strengthening care workers’ rights and voice in the workplace.
1 Introduction
The UK’s adult social care sector has for a decade or more been in a state of crisis (Bunting, 2020; Dowling, 2021). A long history of under-valuing care work has combined with policies of austerity to starve the system of adequate funding and create the conditions for endemic low pay for care workers. This backdrop has then been exacerbated by Brexit and Covid-19, creating catastrophic workforce shortages (more than 105,000 vacancies were reported by Skills for Care in 2020/21 (Fenton et al., 2021)). On access to care, Age UK estimates that there are around 1.5 million older adults with some level of unmet need (Age UK, 2019); this number likely grows if we include missing care for younger adults with physical and mental health needs and learning disabilities, although estimates for these groups are difficult to come by (Forrester-jones and Hammond, 2020).
Despite this precarious position, around 10% of revenue is leaking out of the sector each year in the form of directors’ fees, shareholder dividends, interest and rental payments (Kotecha, 2019). This leakage is, in large part, due to the financialisation of care. Over the last 30 years, the adult social care landscape has changed dramatically, with the number of publicly provided residential care beds falling by 88% from 1980 to 2018 (LaingBuisson, 2018). The private sector has absorbed the majority of these lost beds, accounting for around 84% of the market (by number of beds) by 2019 (Blakeley and Quilter-Pinner, 2019). Most notably, approximately 12% of care beds are now in the hands of investment firms, including private equity, hedge funds, and real-estate investment trusts (REIT), among others (CQC, 2022). Investment firms are drawn to the sector for similar reasons: an aging population with growing needs, asset rich care providers, and guaranteed government funding. However, they differ in the extent to which they are directly involved in running the care home services and the length of time that they intend to stay invested.
Many of the investment firms who have taken over adult social care services employ financial engineering tactics such as debt-leveraged buyouts, asset stripping, and the offshoring of profits (Corlet Walker, Druckman and Jackson, 2022). These strategies tend to be aimed at achieving one of three things: 1) extracting a one-off, large sum of money from the business; 2) extracting cash from the business on an ongoing basis; or 3) increasing the value of the business so as to secure a windfall when the business is sold on (Corlet Walker, Druckman and Jackson, 2021). The drawback of such approaches is that pursuing these goals can sometimes compromise other factors, such as quality of care (Gupta et al., 2021), economic and operational sustainability (e.g. debt-leveraged buyouts are associated with a higher risk of company insolvency (Ayash and Rastad, 2021)), transparency and accountability (Kotecha, 2019), value of money for the taxpayer, and/ or working conditions (Horton, 2019). The potential implications of these risks have been exemplified by the high-profile collapses of two of the UK’s largest providers—Southern Cross and Four Seasons Health Care—in the last decade or so.
In this report, we explore what the challenges associated with financialisation look like within the UK’s care sector. We analyse qualitative data that was gathered through interviews with care workers who worked in residential and nursing homes during, or shortly after, a change of ownership. We look specifically at residential and nursing care for adults over the age of 18—including care homes for individuals with learning disabilities or mental health needs, as well as elderly care—with a primary focus on care workers whose care homes were taken over by investment firms. Our exploratory, qualitative approach to this task reflects both the dearth of literature looking at these dynamics in a UK setting, as well as the lack of available quantitative data on clinical outcomes, care quality, staffing, working conditions and price. The remainder of this report is structured as follows: Section 2 will briefly review what we know so far about how investment firm ownership affects key outcomes in the care sector. Section 3 will outline our methodology for collecting and analysing our data. In Section 4, we present the results of our thematic analysis. Section 5 looks at pay disparities and key performance indicators in fifteen of the UK’s largest care home chains. Finally, in Section 6, we discuss how our analysis builds on the knowledge laid out in Section 2, and we offer a series of policy recommendations for the sector, moving forwards.
2 Background and project aims
There is a small but targeted body of literature that uses statistical approaches to investigate the impacts of financialisation on care. This research predominantly focuses on nursing homes in the United States, thanks to the rich quantitative data available there. For example, national reporting of nursing home deficiencies was first established in the US in 1998. Nursing home report cards now include a raft of indicators on clinical outcomes, staffing levels, and health or safety breaches, and are published on the national Nursing Home Compare website—a site managed by the Centres for Medicare and Medicaid Services (Tamara Konetzka, Yan and Werner, 2021). This is in contrast to the UK, which has a more limited range of data available for such analyses. The Care Quality Commission (CQC), established in 2009, publishes its inspection reports; however, these are largely categorical and descriptive in nature, and do not include systematic data on clinical outcomes.
Studies from the US report a mixed picture in terms of the impact of investment-firm ownership on outcomes in the nursing home sector. Some find that homes with private equity owners have lower levels of staff per resident, lower-skilled staff on average, and higher numbers of incidents of deficiencies, as compared to other firms (Harrington et al., 2001, 2012; Pradhan et al., 2014; Gupta et al., 2021). By contrast, others found no difference in quality (Stevenson and Grabowski, 2008; Huang and Bowblis, 2019). These studies differ in what factors they pay attention to, and which they omit. To our knowledge, the most comprehensive analysis to date has been conducted by Gupta et al. (2021). The paper finds substantial impacts, with a 10% increase in resident mortality associated with private equity ownership over the short-term.
A general limitation of these quantitative studies is that they are largely dependent on the scope of publicly available data sets and may therefore be missing or neglecting key pathways to impact. To better understand the full range and depth of the impacts of investment firm ownership, more exploratory approaches are necessary. In pursuit of this, Bos and Harrington (2017) used a single case study chain to ask: “what happens to a nursing home chain when private equity takes over?”. The authors combined a range of data sources, from interviews with investors, care company executives, and lawyers, to press releases, litigation reports, and indicators of financial performance and resident well-being, among other things. They found that the private equity owner used specific strategies, including low staffing levels, debt-leveraging, re-branding and corporate re-structuring (including separating the property and operating companies in what is known as an ‘op-co prop-co split’). This study highlighted the importance of considering which strategies might be responsible for generating poor outcomes, rather than focusing on ownership type per se.
Burns, Hyde and Killett (2016) was one of the first papers to take such an exploratory approach for the UK, using data from 12 case studies in the post financial crisis period to understand how job quality and care quality are related within nursing homes. Looking at the financial pressures on care organisations after 2008, the authors highlight that care companies at the time needed to manage budget deficits, leading management to “demand more of people at work, as organizations look[ed] to their workers to do more with less” (Burns, Hyde and Killett, 2016, p. 992). They found that the two private equity owned care homes were facing “intensified” financial pressures as a result of the specific financial engineering strategies used by the investors, resulting in “cutbacks in the catering, maintenance, and staffing budgets”. Staff in one of the homes reported that they regularly worked short-staffed, that managers were under pressure not to bring in agency staff and that there were often medication mistakes by nurses (Burns, Hyde and Killett, 2016, p. 1008).
Building on this work, Horton (2019) undertook a series of 25 interviews with investors, industry representatives, regulators, union officials and care workers in private equity owned homes in the UK. Horton (2019) found that, on top of lower wages than the industry average and prolonged pay freezes, care workers also reported that investment firms were reducing sick pay and overtime pay. Further, they reported cuts to activities programmes, and some even spoke of being unable to “obtain basic equipment” such as commodes or sanitary pads (Horton, 2019, p. 9). Through these interviews, the author begins to shed light on key dynamics within the sector, including: how the sense of responsibility of care workers acts as a “source of value” to investors; how investors’ strategies for increasing profitability impact on workers and residents on-the-ground; and how care workers ultimately “complicate efforts” to raise the level of profitability of the company by, for example, refusing to ration key care supplies (Horton, 2019, p. 11).
These papers have begun to reveal what happens within care homes when investment firms take over. However, the literature is still new, and the existing papers are understandably limited in their scope. We therefore aim to take a more comprehensive look at the issues raised in previous works, asking the core research question:
What happens to quality of care and working conditions in UK residential and nursing homes when investment firms take over?
This report builds on existing knowledge by focusing largely on the experiences of care home workers and managers (rather than other actors within the care ecosystem) when their care home is taken over by an investment home. We also include the experiences of those working with adults with mental health needs and learning disabilities, something not widely done before.
3 Methods
The study consists of two core parts detailed below; 1) a set of interviews with care workers; and 2) a review of the financial accounts of large care home providers. Ethical approval for part 1 of this study was granted by the University of Surrey ethics committee. We give a brief overview of the methods used below, with a full methods description detailed in the appendix.
3.1 Interviews with care home staff
We conducted sixteen semi-structured interviews with care staff who were working in residential and nursing home facilities during, or shortly after, a change of ownership, with a primary focus on those who were taken over by investment firms. Prospective participants responded to three recruitment emails sent to a list of members of UNISON (one of the UK’s largest unions) who work in the care sector. We did not tell these individuals that we were interested in investment-firm-owned care homes. This was to avoid eliciting negative rhetoric about the involvement of private equity in the care sector. We felt it was necessary to approach the interviews in this way, given the number of recent high-profile news items discussing the role of private equity in the sector in a negative light. All participants were debriefed following the interview about our interest in investment firm ownership.
Table 1 | Participant characteristics and ownership types (verified using Companies House financial accounts and official statements from the company owners)

Table 1 is an anonymised summary of our participant data. In total, we interviewed sixteen care workers, fourteen of whom were working in the care home at the time it changed hands, and twelve of whom were working in a home that was owned by an investment firm. Where it is of interest, in the write up of our themes we highlight differences/ similarities between the experiences of participants under different types of ownership.
We conducted semi-structured interviews online, which lasted approximately one hour each. Participants were asked a mix of open-ended questions about their experiences of changing ownership in their care home. The data were transcribed, anonymised, and analysed using thematic analysis. This analysis involved attaching detailed codes to each chunk of data, according to their meaning. These codes were then grouped into themes which represent patterns of shared meaning in the data (Braun and Clarke, 2006). Our findings do not tell us about the prevalence of the issues uncovered within the sector. However, what they do tell us is that the issues and dynamics highlighted exist, and they can offer us insights about what processes are driving poor outcomes in the sector.
3.2 Review of company accounts
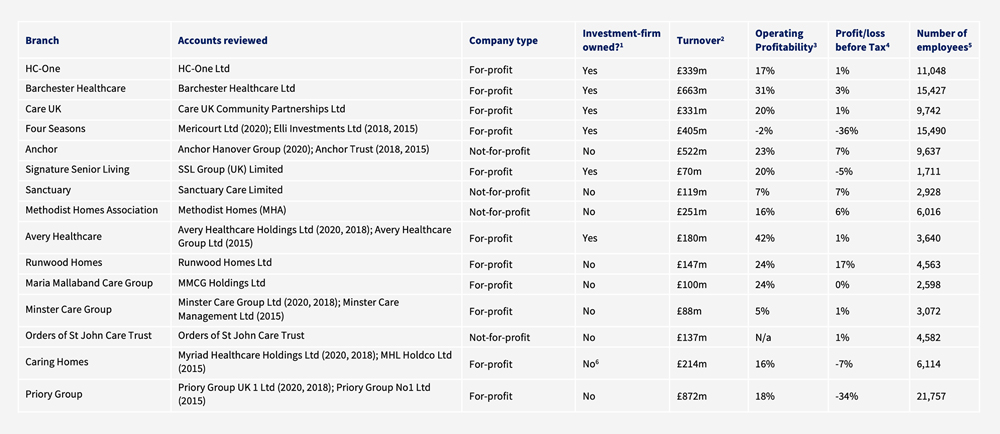
For the review of accounts, we looked at the key business metrics and key performance indicators (KPIs) of 15 of the largest adult social care groups in England, accounting for more than 90,000 care beds between them (approximately 20% of all care beds) by 2022 (CQC, 2022). See the appendix for an explanation of which firms were included and excluded from our analysis. Our final sample consisted of six for-profit groups that were owned by (or had a significant partnership with) an investment firm, five for-profit groups that were not owned by an investment firm, and four not-for-profit groups. See Table 2 for a summary of the companies included in our analysis.
We looked at accounts for the years ending 2015, 2018, and 2020. This allowed us to see changes over time along with differences between those care home groups owned by investment firms, and those which are not. Importantly, the analyses in Sections 4 and 5 were conducted separately and should be read as such. This means that the company accounts discussed in Section 5 will not necessarily correspond to the companies who employed the individuals we interviewed in Section 4.
When analysing the accounts, we focused on two core areas. First, we looked at core business metrics, such as differences in employee and director pay, staff costs, and profitability. This allows us to understand key aspects of business performance for each group.
Table 2 | Key financial information for fifteen of the largest adult social care companies in the UK, as at year end 2020
Second, we analysed key performance indicators. Due to their size, all of the companies studied are required, by law, to report financial and non-financial KPIs as part of their strategic report. The company directors choose which KPIs most effectively measure progress towards particular strategies or objectives, so that shareholders can understand the development, performance, or position of the business. They therefore provide an insight into which strategies and indicators matter most for a particular business.
4 Findings: Thematic analysis
Our thematic analysis of the interview data resulted in the development of the following five themes, which we elaborate in more detail in Sections 4.1 – 4.5 below:
- Exploiting care staff. The first theme we developed through our analysis details the various ways that our participants’ employers exploited them, from reducing staff benefits to chronically understaffing the care home. It also highlights the important role of staff in protecting residents from the negative impacts of this understaffing.
- Cutting corners on service delivery. The second theme builds on these insights, and goes into the range and depth of under-resourcing in the sector, beyond staff shortages. From stories of rationing medical and sanitary supplies and food, to neglecting care home maintenance and failing to deliver enriching activities for residents, interviewees painted a calamitous picture of a care sector that had been stripped back to the bare bones.
- Covering up mismanagement. Our third theme reflects participants’ views that their employer was often mismanaging their care home, and that, in some instances, they were trying to conceal the problems caused by that mismanagement from the industry regulator (e.g., by falsifying paperwork or putting more staff on shift during an inspection).
- Failing to communicate. This perceived mismanagement was compounded by a failure of internal communications—leading to our fourth theme. Interviewees expressed their frustration at the lack of open and effective channels for communication with their employer. They explained how this left them feeling ignored and in the dark about their future and the future of the care home.
- Prioritising profit over care. Finally, we heard from many of our interviewees that they felt their employer was primarily involved in the care sector to make money, and that they didn’t care about the wellbeing of staff or residents. This theme ties together the experiences across the four other themes, revealing interviewees’ perceptions about the motivations behind their employer’s actions.
The themes largely capture care workers’ experiences of how ownership and management decisions impact care services on the ground. Although most of our participants worked in homes owned by investment firms, there were some who did not, or who could compare to other types of ownership before the investment firm took over. Where pertinent we make clear that this is the case. Readers should also bear in mind the self-selecting nature of the study and the pool of participants. Both increase the likelihood that we are capturing more negative experiences than positive. Nonetheless they give us vital insight into what can happen when ownership goes wrong and why.
4.1 Exploiting care staff—“It’s almost like an unspoken ransom”
The accounts of study participants reported in this theme create a picture of care worker exploitation, and appear to represent a systematic attempt by employers to squeeze as much as possible out of each care worker, for as little money as possible. Sometimes care workers said this explicitly themselves, but other times, they simply conveyed the different ways in which the company limited how much they were spending on staff or pressured staff to take on more work, from reducing staff benefits (Section 4.1.1) to chronic understaffing of the care home (Section 4.1.2). Participants also detailed their attempts to protect residents from the negative impacts of these problems (Section 4.1.3). This theme was raised the most frequently by our interviewees, with all sixteen participants contributing to it.
4.1.1 Reducing staffing costs
A starting point for many of our respondents was the fact that staff in the sector feel undervalued and poorly paid. As Emily, a support worker in a care home for adults with mental health needs, put it:
“I think we’re massively undervalued. Massively undervalued. Unappreciated. That’s how we feel. We feel unappreciated.”—Emily
This was raised as a problem for the whole care sector and was sometimes linked to how much local authorities were paying per bed, rather than being an issue that was specific to a particular participant’s employer.
However, building on this baseline of poor hourly pay, many of the interviewed care workers reported that their employers used a variety of tactics to reduce staff benefits. These included limiting or not paying overtime pay, not paying staff for their breaks, limiting holiday entitlements (e.g., by expressing holidays in hours instead of days), reducing staff perks, and limiting pay progression.
The care workers we interviewed often contextualised the inadequacy of their pay and non-wage benefits by contrasting it with the high degree of difficulty and responsibility associated with the job. This was particularly the case for those working in care homes for adults with mental health needs or learning disabilities. For example, Emily spoke about some of the challenging situations she is placed in as a support worker in a mental health facility:
“When someone is in a crisis… if they want to kick your head in and do serious harm, they will. There are a few times we’ve had to dodge the microwave and other things getting thrown. Oh yeah, it has been quite hairy at times.”—Emily
She later went on to say:
“I love my job. Where I work, I absolutely love my job, but I don’t love the pay. I think the pay is horrendous for what they’re expecting me to do and for some of the situations we get put in. I think it’s disgusting.”—Emily
This feeling of disparity between the challenging nature of the job and the limited financial reward was echoed by Robert, a support worker for adults with learning disabilities, who commented:
“Yeah, I mean, like if the wage doesn’t meet the stress that you experience on a day-to-day basis, it’s not worth the job, you know what I mean. Like it’s not hard logic to follow.”—Robert
Beyond the often physically challenging nature of the job, some emphasised the legal and personal risks taken on by many care workers, in the form of administering drugs and completing medical paperwork.
“You go to prison if you give them meds out wrong.”—Will
4.1.2 Chronic understaffing of the care home
Understaffing was another issue that was raised repeatedly by all participants in our sample, with several arguing that the understaffing was an explicit choice by their employer.
“They’re not actually interested in the staffing levels because they say it’s adequate for the amount of residents; that was policy at the heart.”—Michael
Care assistant Laura said that management had repeatedly told staff over the course of her three years at the company that “no matter how many staff we get we’re still going to be understaffed, and that we just have to work smarter rather than harder”. It is difficult to be sure exactly what was meant by this (seemingly illogical) statement without speaking directly to the manager in question, but it could be read as a pragmatic resignation on the part of the manager to the fact that their employer is unwilling or unable to hire enough new staff that current employees would not feel overworked. Training facilitator James went as far as to say that his company’s claims about staffing levels were “nonsense”, and their assertions that they don’t unduly pressure staff were untrue; “in practice they’ll be cracking the whip”.
“If you were interviewing a manager here they’d be telling you, ‘Oh no, no, no, we don’t put any time restraints on them, oh no, no, no, that’s not person-centred care.’ Okay then, so you’ve got two members of staff looking after 24 residents and they’re off for 40 minutes [with a resident] … where’s the cover?”—James
Participants in our study reported numerous consequences associated with this kind of understaffing, from having to deal with too many residents per staff member to not having time to take breaks or drink and eat on shift. Susan, who manages an elderly care home, recalled how she was “literally running” between residents.
One care worker told us that in some cases residents had strict staffing requirements, as prescribed by their ‘care package’. This meant that the care company was prohibited from reducing staff ratios for these residents.
“The staffing… had to stay the same because of the complex people that we look after. So, their packages ensured they were given so many hours one to one, and they couldn’t take staff away if you get what I mean.”—Isabelle
Where it was not possible to reduce staff to resident ratios, employers often seemed to rely on the willingness of the full-time staff to pick up extra shifts. Laura felt this was in place of hiring more full-time staff or using expensive agency and bank staff.
Another key impact of understaffing mentioned throughout the interviews was that staff were having to take on extra jobs around the home (e.g., additional care responsibilities and paperwork, housekeeping and maintenance). One participant explained that the housekeeping staff in the care home (who were often ex-care-workers) were sometimes roped into doing care work when they were very short-staffed.
“They just tell the cleaner, ‘right, you’re caring for the day’… they seem to think it’s acceptable and they do it on a regular basis.”—Michael
Senior carers and deputy managers also reported picking up additional caring duties to support carers when the home was understaffed. For example, Lisa (deputy manager at a home for adults with learning disabilities), explained that because of staffing shortages she was doing “support work at night and management work during the day”. Rebecca told a similar story of having to work on the floor as a care assistant after finishing her medication round because the care company had failed to hire enough appropriately experienced staff for the job.
Beyond expanded care duties, Emily clearly detailed the extent of the extra workload some care workers were having to manage on top of their care duties (similar stories were repeated by several other participants).
“They took away our maintenance man… And we’ve got to do maintenance checks now. We have to do water temperature checks… legionella checks, the bath hoist… the hospital bed that we’ve got. I have to do maintenance checks on the minibus, I’m not even a mechanic… The smoke alarm, we’ve got to go around checking all them… All of them is extra paperwork that we’ve got to do as well… It’s just saving them money, isn’t it?… We’re still trying to give the same amount of care and the same level of care, but we’ve got all these extra[s] in our job role, even though my official title is mental health support worker, it should [be] maintenance worker, activities worker as well, cook as well, you know.”—Emily
4.1.3 Staff protecting residents
Instances of workplace hostility were raised by nine of our study participants. These ranged from rudeness and a lack of empathy, to shouting and swearing at staff members. Respondents also reported management giving staff the impression that they are replaceable, or even actively trying to force them out of their job role, in an attempt to discourage complaints. This perception of general hostility from management and/or the company was compounded by a fear from staff of being blamed for low quality care or for safeguarding issues.
“You don’t see these people and then all of a sudden they will swan in and they’ll point fingers at ‘Well you’re not doing this right and you’re not doing that right’.”—James
“We have safeguarding situations now a lot and again in this I am afraid because one time I could be blamed that I did something wrong and so… very often I am staying after my shifts, for example, 3-4 hours to fill in all documentation properly because I know if [the] documentation [is] not done I could be blamed.”—Rebecca
In the context of these challenging working conditions, participants reported that staff (and sometimes local care home managers) were acting to protect residents from the negative impacts of understaffing and service cuts. They expressed in different ways that the residents were their main concern, and that they would do what they felt was right, even if it was to their own detriment.
“First and foremost, the client comes before anything, it comes before anything else to do.”—Michael
This manifested in a number of ways, with some participants saying that they would rather any extra budget go towards food for residents, instead of staff perks or pay, whilst others put themselves at risk of being disciplined in order to provide the support they felt was needed by the residents. Others still spoke about how they tried not to allow under-resourcing and hostility from management to impact on the quality of the care they were delivering.
“It was only down to the staff themselves that the residents [didn’t] feel the impact more.”—Susan
And some participants even gave examples of staff reaching into their own pockets to make up for service shortfalls; for example, by bringing in food or toiletries for residents, or making financial contributions.
“I know they get so [and so] much allocated from the company, but what we do, it like tops it up a bit, so like we can afford to get them, like, Christmas presents and stuff.”—Emily
Two of our participants articulated that the willingness of staff to put the wellbeing of residents first was being knowingly exploited by their employers.
“That’s what I think [the company] use so much of… the caring factor of the individual [care worker] who cares for those [residents], and it’s almost like an unspoken ransom, you know, ‘Well if you leave what’s going to happen to [the residents]?’”—Lisa
From this quote, it seems that Lisa believes that her employer knows full-well what they are doing, and is taking advantage of the fact that workers care about the residents and would rather be exhausted and overworked than see anything bad happen to them. This commitment to residents is perversely acting as a source of value for employers, potentially enabling them to enact deeper cuts to servicers than they otherwise would, without immediately and adversely affecting quality of care.
“I’m one of them that always helps with staffing, because we don’t have staff. I don’t have to do it. But I said, I’m that type, when they ring, I feel bad to say ‘no’.”—Sarah
The impacts of a hostile work environment and of chronic under-resourcing and understaffing were felt keenly, with several participants reporting that staff were becoming ill with stress and that staff morale more generally was suffering under the strenuous working conditions. It is in this context that some of our participants reflected on the lack of support for staff from their company, and explained that they had to look after one another instead.
“The staff morale just went. It’s just non-existent now. They’re basically turning up to work to make sure they get paid at the end of the month.”—Jennifer
4.2 Cutting corners on service delivery—“They had choices to make, budgets to respect”
We developed this theme by identifying instances in the transcripts where participants had spoken about issues with sub-par service delivery; in particular, where they felt that tight budgets had resulted in corners being cut. Across the interviews, budget constraints were reported to have impacted on staffing levels (Section 4.2.1), medical and sanitary supplies (Section 4.2.2), quality and quantity of food for residents (Section 4.2.3), timely maintenance of equipment and the built environment (Section 4.2.4), and access to enriching activities (Section 4.2.5). All of which participants felt was detrimental to the quality of care and service delivery they were able to provide to residents. All sixteen participants contributed to this theme.
4.2.1 Staff
When asked whether staffing shortages were impacting quality of care, a couple of our interviewed care home workers were adamant that the difficult working conditions didn’t affect the care they were delivering. However, this sentiment was far from universal, with many explaining that under-resourcing was preventing them from being able to spend as much time as they would like to with residents, or deliver the care they felt they should.
“We have to skip some stuff, because it’s just two people. Two people cannot do four people’s jobs.”—Sarah
Concerns over how this under-resourcing was impacting patient wellbeing and safety were also prevalent among interviewed staff. Jennifer, who worked as a senior carer in an elderly residential home, recalled how patients had to “sit wetting themselves” because of the lack of available staff within the care home. She also raised concerns that medication wasn’t being delivered in a timely way because the senior carer was having to deal with too many residents.
“All the medication is all hit and miss. There’s one senior doing all three floors so she’s probably giving out medication for at least 45 people. All the timings will be out.”—Jennifer
In the extreme, James explained his experience of delivering end of life care under poor staffing conditions:
“This is going to sicken you now so be warned—you’ve got to get to the stage that, irrespective of how responsive you’ve been to a resident who’s really failing and who’s coming up to the end of their life, only then right at the very end of this do you get a response, do [the company] put an extra member of staff on maybe for half a day, and you’re sitting there going, all this would have been prevented.”—James
4.2.2 Medical and sanitary supplies
Participants often reported that access to adequate medical and sanitary supplies and equipment was lacking. For example, Michael (a senior care assistant at an elderly care facility) explained how his employer “point blank” refused to buy an appropriately sized bed for the larger residents in the care home, while others spoke about restricted supplies of sanitary pads and personal protective equipment.
“Even pads, they would tell us ‘We are on a budget. You have to use one pad a day’.”—Sarah
In the eyes of our participants, such restrictions were detrimental to the quality of care they were able to provide to residents. Laura even felt that the rationing of surgical masks had caused higher rates of Covid-19 infections within her care home.
“We lost a lot of people over it, a lot of people we shouldn’t have lost.”—Laura
4.2.3 Food
Six of our study participants spoke about the poor-quality food that was being provided for residents. Michael lamented the fact that all the food the residents receive is cheap and mass-produced.
“There’s no nutritional benefit in it, it’s just crap. It’s that bad right, that staff will bring cakes and things in for tea.”—Michael
Meanwhile, Jennifer emphasised the knock-on effects this has on residents’ broader wellbeing.
“When you’re hungry you’re agitated, so if you get hungry people at night they’re not sleeping properly because they’re hungry.”—Jennifer
Senior learning assistant Amanda felt that these kinds of food budget restrictions were a result of the goal of the service “to be profitable”.
“That was the aim of the service quite clearly and because of that… they had choices to make, budgets to respect and that would have had an effect on everything in the running of the house.”—Amanda
James was particularly concerned that money was going to managers’ bonuses and “leakage” to offshore companies, rather than being spent on improving the food provided to residents.
“When you start to know all about the leakage, we could feed our residents much better, we could have more staff in there, not a problem.”—James
4.2.4 Equipment and maintenance
A number of our participants complained that their houses were run-down and felt that budgetary constraints were driving underspending on maintenance and equipment replacement in the care home.
“Now they’re saying they’ve run out of money, and we’re not allowed any repairs unless it’s an emergency until April.”—Emily
Amanda spoke about the long wait times to get things fixed, comparing these problems starkly to the approach of the previous owner who did weekly maintenance checks around the home and fixed problems quickly. David also spoke about proactivity with regards to maintenance as an important part of ‘good’ ownership.
“The amount of times that we said we need things fixing… the tumble dryer’s broken, needs fixing, [the] washing machine needs fixing, the dishwasher needs fixing. You know, household things that are important on a daily basis… I personally raised a problem that has been there since I started working in 2015, that was the dishwasher. Simple things that you would think all it takes is one person to go and buy a new one and fit it in, simple as. Five years down the line, still a dishwasher that doesn’t work.”—Amanda
Throughout the interviews, a particular framing of these budgetary issues cropped up a number of times. Participants explicitly contrasted the size of the salaries and profits that people in the upper management/ownership of the company were taking home with the degree of under-resourcing of things that were deemed fundamental to service delivery. Care home manager Isabelle captured it well:
“I was disgusted, if you like, because the care home is in a pretty poor state of repair, and it’s really evident. If you were a guest here today, you would think oh my life, how are these people living and working in these conditions. So, when [the new company] came with all… their flash cars and their nice clothes and their big houses and fancy holidays… I mean I’ve got doors here that blow open, French doors that blow open in the strong winds, because they’re just not fit for purpose. It’s shocking that, you know, they live that lifestyle, yet the service users don’t have a nice home and that really upsets me.”—Isabelle
4.2.5 Activities
Finally, a number of participants bought up a lack of access to enriching activities. Each of them felt these missing activities were important for residents’ overall wellbeing, with Robert and Lisa both highlighting how the small “almost intangible things” (Lisa) can make a difference. Speaking about the service under the old ownership, Robert felt that they did more activities with the residents, and that they would “go out and actually make an effort to, you know, have a nice day”. Meanwhile, Michael had a particularly jaded view of the implications of missing out on a broader approach to care, comparing his care home to a “prison for pensioners”.
“It’s just basically containment and just wait for you to die and we’ll get somebody else to fill your room.”—Michael
4.3 Covering up mismanagement—“I think [they] have no idea how to run a care home”
This theme captures participants’ feelings that their employer was mismanaging their care home (Section 4.3.1), and that they were more interested in how the care home looked to families and the regulator than they were in the quality of the care being delivered (Section 4.3.2). Given the self-selecting nature of our study it is unsurprising that many of the people who came forward to take part in our interviews felt that their employers were not offering the kind of care or working conditions they would like to see. Indeed, many of the interviewed staff felt that their employers were making poor decisions about how to run their care home.
“I think [the company] have no idea how to run a care home… I think anywhere that has that [company] motif, I don’t think it’s right good.”—Jennifer
Examples of employer-incompetence recalled by our participants included: hiring staff and managers who were inexperienced or unqualified; pressuring staff to take on residents who were not suitable for their particular care home (e.g., due to extra medical needs); and implementing inappropriate policies and procedures for their type of care home (e.g., an unnecessary activity-based checklist for adults in supported living who have full capacity). We discuss several of these examples in detail below, focusing in particular on incidents where mismanagement was framed by participants as being deliberate and motivated by the financial aspirations of the employer.
These issues were also communicated by those working in small, privately owned companies, with more of an emphasis on the owner behaving in a hap hazard or renegade fashion: “He was a bit of a wheeler dealer” (Isabelle). However, in these cases, both participants were managers and both reported being more able to retain control of the day-to-day running of the business than those participants from larger, investment-firm-owned care chains.
“He had no say in the day to day running of anything because he didn’t really know what he was talking about. So, I wouldn’t have had that respect for him if he had even tried.”—Isabelle
4.3.1 Care home mismanagement
First, several participants raised the fact that their employer was hiring inexperienced or poor-quality staff. Michael spoke about his frustration that his employer would bring in agency staff who “don’t know the lay of the land” and who, as a result, were making a substantial number of medication errors. Exasperation at poor staffing policies were echoed by other participants. Rebecca, for example, who is also an elderly care senior care assistant, commented that it seemed her employer thought they could just hire anybody and “everything will be okay”. She immediately reflected: “it’s not like that”.
“It’s very stressful, plus agency staff they are not confident with our company’s documentation and some of them [are] refusing to fill it [in], which means I need to it.”—Rebecca
These could be straightforward examples of poor hiring decisions by care providers, potentially reflecting the difficult recruitment environment in the UK care sector[7]. However, they might also be examples of employers intentionally hiring cheaper labour, without due concern for the consequences on permanent staff and residents. In the case of agency staff, they can in theory work out cheaper in the long run than hiring additional members of full-time staff, if they are used sparingly to fill staffing gaps. This is because, although their hourly rate is higher than full-time staff, the employer doesn’t have to cover expensive annual overhead costs.
Concerns about poor hiring decisions also extended to management positions. Several interviewees offered examples of a new employer putting in place management who were unqualified and who lacked the required knowledge about how to do their job effectively. When talking about a manager who was unable to explain basic hygiene regulations, James quipped: “£98,000 a year? You must be mad”. Similarly, when speculating on the reasons behind hiring a manager with “no qualifications”, Jennifer, who worked as a senior carer in an elderly residential home, felt that there were ulterior motives at play, with the employer trying to cultivate a certain reputation for the care home.
“I think they’ve just got her in to make it look good.”—Jennifer
A second example of perceived mismanagement was the general disregard from some employers for the nuances of choosing which types of residents to take on. Some participants reported pressures from above to take all and any service users, even if they were a poor fit with other service users already living in the home, or if their needs were too great given the available resources. Support worker Robert, who works with adults with learning disabilities, recalled how his care home had taken on a service user who “didn’t mix in with the other service users too well”, and that the upper management were “pushing to just fill this bedroom”. Others also framed the lack of attention to resident dynamics as being motivated by a desire to fill beds and maintain high occupancy levels.
“If we could not fulfil that man’s requirements then that man should’ve went to some place that did and that’s a nursing home; you’d have extra staff, you’d have everything else. We couldn’t fulfil his requirements. We didn’t fulfil his requirements for months… That’s down to management then to turn round… forget about the bum on the bed, because that’s what it was. This is my estimation. So much more could’ve been done for that man.”—James
Third, a number of our participants had experienced owners who were new to their sector. For example, Will—a support worker for adults with learning disabilities—spoke about how his care home was the first learning disability service that his charity had run, and how the owners were investing large amounts of money into trying to ensure that it didn’t fail.
“They are absolute[ly] adamant they need this to work because it’s their flagship, otherwise we would have got handed back [to the local authority].”—Will
For Isabelle, the inexperienced owner meant that her residential care service had been given blanket policies and procedures that “were really for domiciliary care and supported living”. She spoke about how she wished she had an owner who “knew about the care field”, who took “an interest in the service users” and who helped “to progress the service”. These comments portrayed an image of an employer who had little interest in the care being provided in the home. Similarly, Emily saw her mental health service “voted down by CQC” (Care Quality Commission) as a result of the incorrect paperwork that was put in place by the new owner. Both participants felt frustrated that their employers’ involvement in the sector seemed to be largely financially motivated, with little interest in staff and residents.
“The staff morale dipped big time because we were perplexed as to why this company has taken us over and they have no, well very little understanding of mental health. So, they saw these figures and thought ‘oh we can make some money there’ and they bought our company. So, it was, like, okay thanks.”—Emily
A final aspect of mismanagement raised by participants during the interviews was the general lack of vision for the future of their care home from their employer. Using the example of the digital development of the company, David, who works with adults with learning disabilities, compared the more proactive “adapt and sustain” approach of his care home’s new owners to the approach of the old owners, who he described as taking the attitude “Okay, whatever comes let it come”, with no long-term plan for adaptation and development. Frustration at the lack of long-term planning at the level of the individual care home was mirrored by others.
“If you leave a complete floor that does require refurbishing, equipment put in place, etc, etc, and it’s been lying there, dormant, let’s say for the last five months, six months, doesn’t that make it worrying?… For me that doesn’t give an indication of having any sense of direction or how you’re going to take the home forward.”—James
4.3.2 Covering up the problems
Many participants spoke about a preoccupation with hitting KPIs and targets and making the care home look good to families and the CQC, rather than delivering the best possible care to residents. A number of participants told us about how their employer was asking them to prioritise paperwork over care delivery and, in one case, to even falsify paperwork to make it look like the care home was delivering better care than it actually was. While some acknowledged the importance of paperwork from a safeguarding and accountability perspective, many still felt that it wasn’t portraying a true picture of what was going on in the care home.
“It’s… not correlating to how we actually are.”—Laura
Because this extra paperwork was often not coupled with additional resourcing to give care workers the time to do it, some of our interviewees argued that it added to the pressures of the job and even took time away from being able to do the care-focused parts of their job.
“It’s the swan theory, isn’t it, you know, we’re gliding along the water, but our feet are going like the clappers underneath because that’s the truth of it. You know, yes, we’re under pressure with everything else, we will try and provide the paperwork to meet the goals, to meet the quality, to meet the financial audits, etc, but we’re just frantically swimming like hell underneath to do it all.”—Lisa
Indeed, several of the interviewed care home workers felt that the focus on paperwork was more about covering the backs of staff and management if anything goes wrong, rather than being about ensuring quality. Sarah, who is a care assistant at a residential home, even recalled being asked by the care home manager to lie on her paperwork, to say that she had turned a resident in their bed (to avoid pressure sores) every two hours, even if she hadn’t.
“When I say, ‘Why?’ They say, ‘It covers our back’. That’s what they say. And I just drop my pen, I say, ‘I’m not writing it. I didn’t do it.’”—Sarah
Participants also spoke about other strategies aimed at putting on a show for the Care Quality Commission whenever they inspected the home. These strategies ranged from adding extra agency staff on shift to “make it look busy” (Michael), to removing staff members “who are very outspoken” (Sarah) from the rota when the CQC inspectors were due. These stories were often immediately contrasted with a reflection on how the care home went back to normal staffing levels straight after the inspection.
“When I was in the other day, we were that understaffed the manager was having to mop the floor.”—Thomas
By coercing staff into covering up the aspects of care provision that are falling short of the expected standard, Sarah felt that the situation was being enabled to continue.
“My home manager said, ‘Oh, we passed the CQC, that was a surprise.’ So, I was [also] surprised, because there were things that were still wrong. They were still wrong, wrong, wrong, wrong, wrong.”—Sarah
4.4 Failing to communicate—“I don’t trust them, and I don’t think they’re being honest”
This theme describes the disconnect between those living and working in the care homes, and the upper management of the company, characterised by poor communication (Section 4.4.1) and a lack of transparency from participants’ employers (Section 4.4.2). This includes participants’ accounts of difficulties in communicating feedback to the company and affecting change within their workplace, as well as their impressions that the company is disinterested in the care home, with some reflecting on how infrequently upper management would set foot in the home. All told, the lack of effective channels through which staff could communicate their needs and issues left participants feeling ignored and disempowered.
“We felt that we were completely left out, ignored.”—Amanda
This, combined with a lack of transparency, led some of the interviewed care home staff to distrust their employers: “I don’t trust them, and I don’t think they’re being honest” (Isabelle); with Lisa likening her employer to the suspicious company at the centre of a murder mystery TV series: “people know things; things have happened that nobody talks about”.
4.4.1 Poor communication
Many study participants reported a general sense of distance (either physical or metaphorical) between the upper management and the staff and residents in the care homes. Some spoke about their perception that the company was completely uninterested in what was going on in the care home.
“I had no personal relationship with like the upper management. They never really came in to talk to the staff… There wasn’t even like meeting with the upper management. They were just up in the office all the time. Like they never came onto the floor… if ever.”—Robert
A number of others emphasised the very physical process of isolation, with their unit manager becoming progressively more closed-off after the new ownership took over.
“Within that time, in service as line manager, they have gradually become more and more detached from staff as if in less around the house, more closed into their office, door closed, in constant meetings, constantly busy.”—Amanda
In an extreme case, Rebecca said that her new manager remained hidden away in the administration building, telling us that “for three months some of us had no idea how she looked”. Care home managers occupy a unique position within the social network of care home companies, operating as gatekeepers that can either facilitate or hinder the flow of communication between care staff and upper management. As such, the physical process of isolation described by Rebecca and others may well have an impact on the perceived workplace autonomy and wellbeing of staff.
“Disjointed, isn’t it? … the chain of command from the top right to the care staff… that link should be strong, the communication should flow both ways. For the carer staff it’s always one way traffic.”—James
In addition to the sense of distance felt by some participants between themselves and upper management, many of the care workers we spoke to described more generally the limited (and sometimes non-existent) avenues for affecting change within their home. Some recalled their attempts to communicate with management and HR about ongoing issues, saying that they received no real response or action from the company.
“We exhausted every avenue that myself and my Deputy humanly could to get them to understand this wasn’t working, it wasn’t safe and it wasn’t right, you know.”—Susan
Jennifer talked to us about ongoing issues with racism in the care sector, and in her care home in particular, emphasising that the sector did not cater to the haircare, skincare, or food and language needs of people of colour. She tried to secure some training for the staff on these issues but reached a dead end after speaking to her manager.
“She did say she’d look into it, [but] nothing ever came of it because you’re not supposed to have ideas, you’re supposed to just be brain-dead.”—Jennifer
Others echoed similar frustrations around a lack of responsiveness to feedback.
“When we complained that we didn’t have the right equipment, safety equipment for around Covid time, nothing happened… It felt like I was shouting into a void because it may change for like a day or so but it always went back to where it was.”—Laura
Some participants bought up what appeared to be tokenistic offers to give feedback on their care home. For example, Rebecca recalled a time when she had tried to raise an issue with the care home manager. She contrasted the friendly welcoming tone of the email response she initially received, seemingly inviting open communication—“If you have any questions or you want any more information you can come and see me”—to the overtly hostile reaction she encountered when actually following up in person: “they blamed on me and they shouted at me, they shouted in very rude ways”. Other companies sent out anonymous questionnaires to their employees. However, Amanda noted that the issues she raised through the feedback forms were “never addressed”.
“We were saying we actually need things for the young adults, we need things for the people we support… We felt like we were never seeing any of the executive[s] coming into our settings… No one was ever coming to check what was needed fixing.”—Amanda
This left some wondering “what’s the point in saying anything because nothing happens, nothing gets done” (Lisa). As we raised in Section 4.3 above, Sarah—as an outspoken advocate for improving care home conditions—was removed from the rota when the CQC was due for its inspection, further impairing her ability to notify anyone about the poor working conditions.
As a result of the limited channels for communication, there was a ready recognition among many of the participants that they were very far from the decision-making centre of the company, with little to no means to effect change within their workplace.
“I can phone them but it’s very rare you would ever have a meeting with them face to face. Because you’re at the bottom of the food chain, you’re the cogs of the wheel but they’re the seat and the handlebars, do you know what I mean?”—Michael
By closing the channels for formal communication, these care companies are inhibiting workers’ ability to resist exploitation or demand change.
“If I want to talk at the AGM, I have to buy a share in order to be able to say, ‘you’re shit’.”—Thomas
4.4.2 Lack of transparency
Finally, a lack of transparency—sometimes combined with empty promises to staff that their ‘lot’ and the ‘lot’ of residents would improve—came up a number of times as a cause for concern for our interviewees. The transparency concerns ranged from the opaque structure of the company as a whole, with complex corporate group structures that “end up all back, as it is, in Guernsey” (James), to behind-the-scenes changes to staffing contracts. Lisa realised that her employer had been keeping things from the staff when she moved into a management position within her care home.
“We’re subtly having our hours reduced without actually being advised that, you know, ‘Because of restructuring, because of how we are going to run this business, this is what is going to happen, are you happy or unhappy with that?’ You know?—Lisa
Concerns over a lack of transparency were echoed by other participants, most of whom were in management positions. Many of the same participants also expressed frustrations about how upper management would promise “all this, that and the other” (Emily), claiming that they were going to improve conditions within the care home (e.g., new buildings, equipment, etc), but failing to deliver on those promises. James felt that the rhetoric was just empty bluster.
“All you’re doing is you’re standing there trying to blow smoke up [our] arses.”—James
4.5 Prioritising profit over care—“It was all money, money, money”
This fifth thematic cluster reflects the fact that many of our participants felt their employer was much more interested in making money than in the wellbeing of their staff and residents. Some participants spoke indirectly about how their new employer felt very corporate (Section 4.5.1) and/or took little interest in the care home staff and its residents (Section 4.5.2), whilst others were more direct in their assertions that the company was there to make money (Section 4.5.3). The theme ties a lot of the issues from previous themes together, with participants offering the company’s financial aspirations as an explanation for various issues, including understaffing and cutting corners on service delivery.
4.5.1 Corporate style employer
Some participants spoke about how their new employer felt “more corporate” (Susan) whilst others described a top-heavy company structure characterised by large salaries and complex ownership structures. Participants who worked in charities also reported similar corporate-like structures.
“Charities may well be split into two… there will be the care and support element, and another element may well be housing.”—Charles
“I’m only surmising that the founders of these charities are definitely on a lot more money than I am.”—Will
In addition, two participants recalled the use of corporate-style employee incentive schemes, such as flu and Covid-19 vaccination bonuses and “refer a friend” programmes (Emily). The clearest example was a “system of perks”, introduced at Amanda’s care home, that was linked to a weekly feedback questionnaire. Not only did Amanda report that care staff would rather the money for perks be spent on better quality food for residents—“we believe that that is more important than our perk box and all that crap”—but she also highlighted that the perks often didn’t really apply to care staff and were more targeted at people with manager-level salaries. For example, there was a car discount that “was only applying to certain types of cars that were completely out of our budget as care workers”. More fundamentally, she captured the mismatch between these corporate-style incentive schemes and the reality of day-to-day work in a care home:
“You know, a perk box, benefits and all that, is all really nice and it sounds really nice; in reality, it doesn’t really work. It’s not our job, it’s not what we’re doing. We’re looking after people, you know, we’re feeding them, we’re washing them, we’re bathing them, we take them out in the community… This is what we do on a daily basis at Christmas time, Easter time and it’s, we’re not there to fill in a questionnaire online at the end of the week.”—Amanda
4.5.2 The company doesn’t care
Participants also expressed in many ways that they didn’t feel their companies cared about residents or staff.
“Don’t say they all care, it’s all about money and numbers, right, that’s it, that’s it.”—Will
This seemed to extend particularly to the health and wellbeing needs of staff. For example, Thomas spoke to the new company about his disability when they first took over and was told that they had good systems in place to support him, but he never heard anything more from them.
“I feel as a disabled person that the company as a whole don’t give a hoot.”—Thomas
Emily also detailed how the company reacted to her medical needs, saying:
“I was off for four months from Easter, and only the manager actually phoned, that’s because I get on so well with him… but area manager, anyone else from HR or anything, not one message, not one email, nothing. We just feel like we’re just a number basically.”—Emily
She added:
“I am medically exempt from wearing a face mask, but [the company] have stipulated… to the manager that I have to wear a face mask at all times, and if I don’t, I’ll be sent home and I’ll get sick pay for four months and then probably dismissed.”—Emily
This aligns with the accounts of hostility that we summarised in Section 4.1.3, reporting on the exploitation of care staff.
4.5.3 Only interested in money
Most strikingly, many of our study participants spoke directly about how they felt their company prioritised profits over care. Eleven of the interviewed staff said something to the effect of ‘it’s a business’ or ‘it’s all about money’ at some point during the course of the interview.
“I think the reason people come and do this, buy this, and own this is simply to make a profit.”—Isabelle
“It is more about money than the people, definitely.”—Emily
“It’s all about business. It’s all about their profits.”—Sarah
Michael felt that the expectation of a “return on your money” by investors was linked to a workforce strategy of “squeeze and squeeze and squeeze”. This acute awareness by some participants of the role of money and profit in motivating the involvement of their employer in the sector led some to argue that a not-for-profit model of care would be better for residents and workers. However, this would need to be accompanied with broader changes to the structure of the sector because, as Will commented, even his charity employer was in it “to make money” for certain people (e.g., high salaried bosses). Others said that they did feel comfortable with the for-profit element of care delivery to some extent, as long as it wasn’t excessive.
“So with every £100 coming here, there’s £13.95 never gets here and it’s never on the books, it’s never taxed, it’s never nothing… Excuse me because I get really annoyed with these things… See, I understand about capitalism, I mean, okay, you’ve got investors and stuff, that’s fair, they want to make money, that’s fair, however such leakage is disgusting.”—James
When asked about the future of adult social care, many highlighted the potential advantages of taking profit and other large corporate structures such as large directors’ salaries out of the care sector, with some arguing for an National Health Service (NHS) style model, while others preferred the idea of smaller independent charities or cooperative care companies. Participants felt that these models of care would offer a variety of benefits: more transparency, accountability, consistency in what was being offered across the country, better upkeep of buildings, and more staff recognition and fair pay grades. Susan felt that, however desirable, moving towards an NHS-style model was not a realistic goal and felt that we do not have the money, time or power to make the necessary changes.
5 Findings: Review of accounts
In this section we review the accounts of fifteen of the UK’s largest adult social care groups. Our sample consists of six for-profit groups that have an investment firm owner/significant partner, five for-profit groups that are not owned by an investment firm, and four not-for-profit groups. We look at accounts for the years ending 2015, 2018, and 2020. Overall, in 2020 most groups were reasonably profitable with an average of 23% of their turnover remaining as operating profits (i.e., a 23% margin) which was slightly higher than in 2018 (22%) and 2015 (21%) (see Table 2 in Section 3 above). By operating profits, we mean earnings before interest, taxes, depreciation, amortization, and restructuring or rent costs (EBITDAR), excluding exceptional items. This average excludes the five groups where we were not able to calculate their EBITDAR in 2020.[8] Avery Healthcare had the highest operating profit margin across all years, which partly reflects the fact that it has an above-average proportion of self-funded residents who typically pay higher fees.
5.1 Employee remuneration
We calculated average remuneration (i.e., pay including basic salary and any additional payments such as overtime, bonuses, social security costs and pensions) per employee and per director for our sample.[9] Across our sample we found that, from 2015 to 2020, average remuneration per director had grown at almost double the rate of remuneration per employee. This means that by 2020, the average director’s remuneration was 11 times higher than that of the average employee. See Table 3 below.
Table 3 | Change in average remuneration per employee or director from 2015 to 2020 (sample of eleven care groups with comparable data). These figures are an average across all ownership types[10]
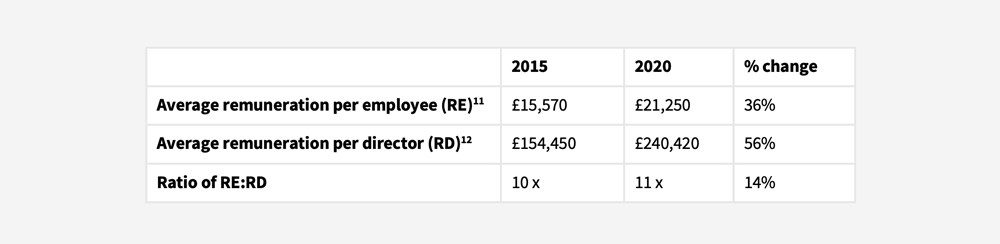
Our findings for average remuneration per employee are similar to those reported by Skills for Care’s adult social care workforce estimates, with yearly pay for a care worker at £20,700 and for a senior care work at £25,700 in 2020/21 (Fenton et al., 2021, p. 95). The differences will be in part because we are only looking at a sample of care companies, not the whole sector, and also because our estimate of remuneration per employee reflects the full cost to the employer, and so includes pension contributions and social security costs. We also calculate pay for all employees in a company below director level and so include higher paid managers and administration staff in the figure too. Additionally, most accounts provided us with average numbers of staff in a year, whilst Skills for Care uses FTE (full time equivalent) annual pay.
When comparing across groups, for-profit care groups owned by an investment firm paid their directors on average more than other for-profit groups as well as not-for-profits, with average remuneration per director (in 2020) at £296,600 for investment firm-owned groups, versus £237,600 for other for-profits that are not owned by an investment firm, and £149,600 in not-for-profits (see Table 4 below).
Table 4 | Average remuneration per employee and director in 2020 (sample of eleven care groups with comparable data)
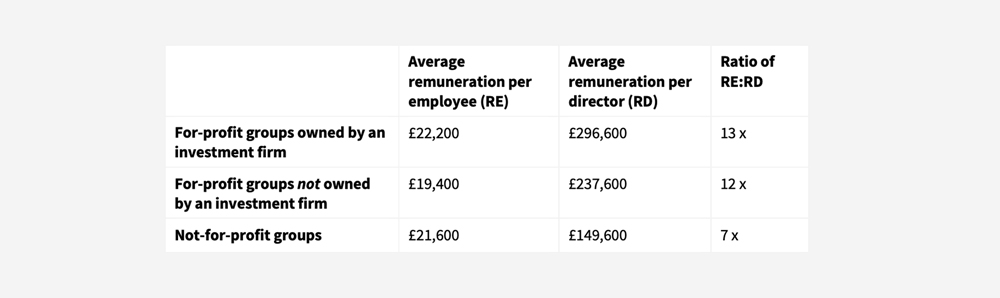
The ratio of average remuneration per director to remuneration per employee has grown substantially between 2015 and 2020 for investment firm-owned groups, whilst it has dropped slightly for not-for-profit groups (see Figure 1). It fell in not-for-profits because remuneration per director grew by only 3% whilst remuneration per employee grew in line with the average at 37%. By 2020 investment-firm-owned groups had a higher remuneration ratio (13 times) than other for-profit or not-for-profit groups. This is because the average director pay was higher in investment firm-owned groups. The discrepancy between the average director’s pay in investment-firm-owned groups and the average in not-for-profit groups was equivalent to the average salary of more than six employees.
Figure 1 | Ratio of average pay per director to pay per employee in 2015 and 2020 (sample of eleven care groups with comparable data)

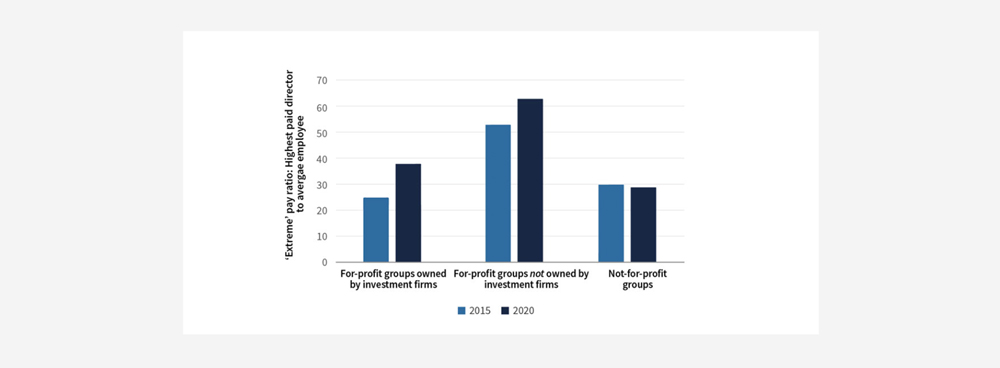
In terms of the ratio of highest-paid director to average employee remuneration, the for-profit groups not owned by investment firms (three out of five reporting) had the highest ratios, with the highest paid director being paid, on average, 63 times more than the average employee in 2020 (see Figure 2). However, this is driven by one company in particular, Runwood Homes, who had a ratio of 165:1 in 2020. The one not-for-profit company that reported its figures had a similar ratio to the investment-firm-owned groups (4 out of 6 reporting) at 29:1 and 38:1 respectively in 2020. This pay disparity grew between 2015 and 2020 for all for-profit groups (including those owned by an investment firm, and those not). It is also worth noting that the yearly pay of a company director in an investment-firm-owned group is likely to be an underestimate in the long-run because they typically receive a large chunk of their compensation upon the successful sale of the business.
These ratios of highest paid director to average employee remuneration are broadly in line with ratios in other large companies. For example, a report from the High Pay Centre in 2020 found that the average CEO to median employee pay ratio for FTSE 350 companies was 53:1 (Kay and Hildyard, 2020). However, they stand in stark contrast to the much smaller pay disparities in the NHS, where the remuneration of the chief executive of the NHS is approximately seven times that of the average employee (authors’ own calculation based on data from Cabinet Office (2021) and NHS Digital (2022)).
Figure 2 | Average ratio of highest paid directors’ pay to pay per employee in 2015 and 2020 (sample of eight groups)
5.2 Key performance indicators
Reviewing all fifteen companies we found that the majority had KPIs in the ‘capacity and occupancy’, ‘income and resident type’, ‘sustainability and profitability’, and ‘cost control’ categories (see Figure 3 below). This reflects the fact that the key profitability drivers in the care industry are occupancy, income, and limiting the impact of cost increases. Indicators monitoring staff wellbeing and training were less commonly included, despite staff being the main input for a care business. Those that did revolve around staff were usually focused on labour cost per bed, hour, or resident; i.e., considering staff as a form of cost to be managed rather than an asset to be nurtured. This attitude was particularly visible during the pandemic when it was reported that some care staff were not receiving sick pay when self-isolating, forcing them to use up their annual leave or risk returning to work early in order to financially sustain themselves (UNISON 2021).
We broke the KPIs down into different ownership groups, finding that investment-firm-owned groups were most likely to have KPIs in the categories of ‘capacity and occupancy’ and ‘income and resident type’ (see Figure 4 below). Within the category of ‘income and resident type’ there were notable differences in the KPIs used by investment-firm-owned groups and not-for-profit groups. The former were heavily focused on the proportion of self-funders and fee rates, whilst the latter focused more on revenue. Similarly, within the ‘sustainability and profitability’ category, there were differences between for- and not-for-profits. For-profit groups (both investment-firm-owned and others) were more focused on KPIs relating to operating profitability, and their ability to generate sufficient cash to pay their debts, whilst not-for-profits focused more heavily on financial sustainability and generating a surplus for reinvestment.
Figure 3 | Number of companies with at least one KPI in each category in 2020
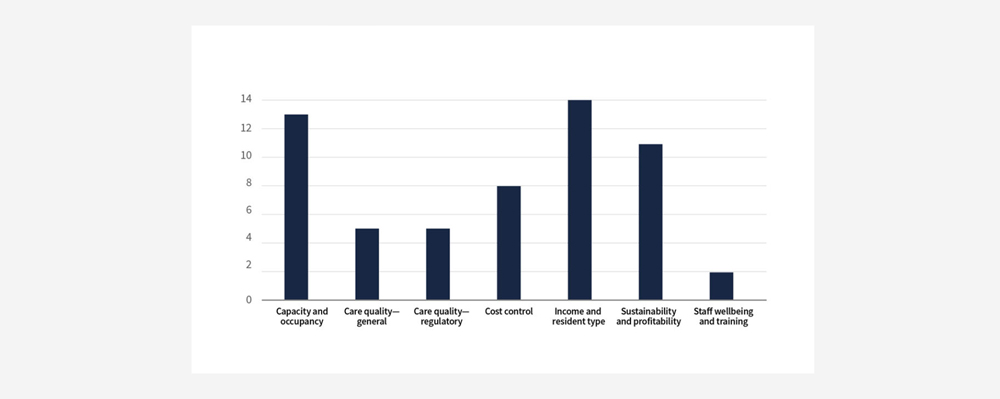
Figure 4 | Proportion of care home groups with KPIs in each category by ownership type in 2020
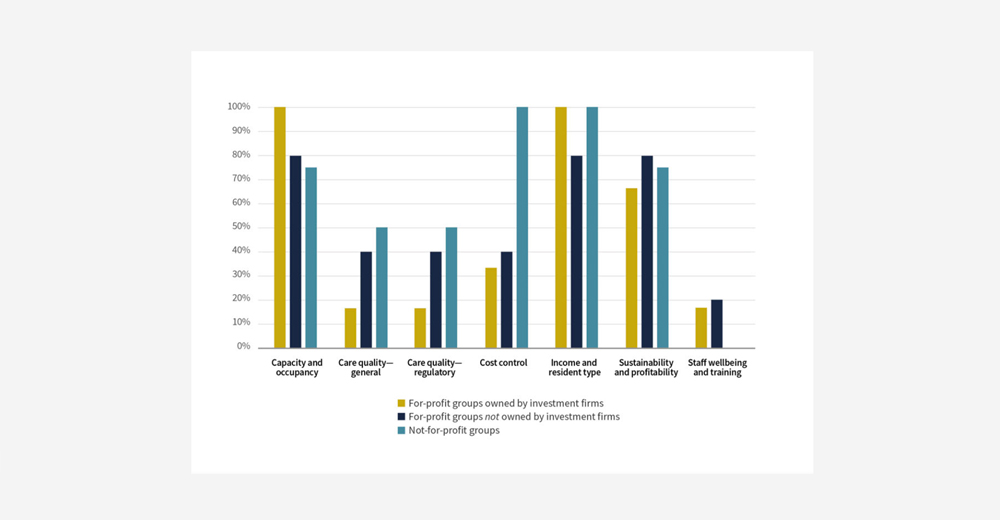
We also found that not-for-profit groups were more likely to have KPIs relating to ‘cost control’. These were particularly focused on monitoring costs per unit, such as cost per resident per week, management costs per unit, and staffing cost per bed. It is difficult to say concretely, but there may be a number of reasons why not-for-profits consider cost control KPIs a key business metric to report on.
First, according to industry analysts LaingBuisson (2021), not-for-profit care groups tend to focus principally on residential homes whilst for-profit groups have a stronger focus on nursing homes. In 2018, they estimate that 73% of all not-for-profit beds are for residential care, whilst 53% of for-profit beds are residential (with the remainder being for nursing care). This is reflected in our sample, with 67% of the care homes in the not-for-profit chains in our sample registered as providing care without nursing (i.e., residential), whilst only 45% of for-profit care homes in our sample were offering non-nursing care (authors’ own calculations based on CQC data as at 1st March 2022). This may impact how easily not-for-profit groups are able to manage the emerging trend towards increasingly complex and costly residents in the residential part of the market.
Under budget pressures, local authorities have favoured providing homecare for elderly residents instead of paying for (usually more expensive) care home places, thus “generating savings” for the local authority (Laing Buisson, 2018, p. 54). As a result, over time, those residents who have been placed in care homes have tended to be those with more complex needs as “some of those who would previously have been placed in residential care are now receiving homecare services” (Laing Buisson, 2018, p. 53). This trend has been coupled with a preference by local authorities to place individuals in residential care homes—which generally have lower fees (LaingBuisson, 2021)—rather than in nursing homes. This has been described as a process of transferring demand “down the continuum of care services” (Laing Buisson, 2018, p. 53). Residential homes are typically less well-equipped to handle the needs and costs of higher acuity residents. This may explain in part why not-for-profits focus more explicitly on cost control KPIs, as a larger proportion of their business may have been impacted by this trend towards higher acuity residents.
The challenge of absorbing the higher costs associated with more complex residents may be even tougher for the not-for-profits groups in our sample for two reasons: one, residential homes have, on average, fewer beds per home than nursing homes (LaingBuisson, 2021), likely limiting their opportunities for economies of scale at the level of the individual care home, and their ability to spread the costs of new equipment and training across multiple residents. The average number of beds per home across the not-for-profit chains in our sample was 51, as compared to 61 beds in the for-profit portion of our sample.
Two, the not-for-profits (and for-profit groups not owned by investors) in our sample tended to be smaller in scale than the investment-firm-owned groups. This matters because it has been noted that larger groups can “exploit economies of scale” by, for example, taking advantage their “greater purchasing power for consumables such as utilities and food” (LaingBuisson, 2021, p. 15). The pressure to generate economies of scale to aid financial sustainability is notable across the sector. For example, the not-for-profit Anchor Trust stated before its proposed merger with Hanover Housing Association that a merger would: “drive down the cost of doing business, and follows several years of efficiency savings”, and that Anchor: “work[s] to mitigate the impact of cost inflation and uncertainty by a process of continuous improvement to drive down our cost base” (Anchor Trust, 2018, pp. 5, 9).
These cost pressures are further exacerbated in those care homes that have a high proportion of local authority funded residents, since they have less flexibility to increase fees in line with the rising costs of care. It’s been noted by industry analysts and the Competition and Markets Authority (CMA) that the price paid per resident by local authorities has, in some parts of the country, not kept up with the costs of providing care (CMA, 2017). For example, the charity Orders of St John Care Trust describe their situation with regards to local authority contracts in the following way: “with rising costs outstripping fee rate increases there is often a gap between the level of fees received and the cost of care delivery” (The Orders of St John Care Trust, 2018, p. 14). This is particularly pressing because, at the time, 61% of their residents were funded by a local authority.
In general, the care industry faces a “continued upward trend” in property, staff and food costs, with increases in staffing cost outgrowing both local authority and private fees from 2016 to 2021, and food costs having risen by 17.2% from 2018 to 2021 (Knight Frank, 2021, p. 10). This explains in part why eight out of fifteen of the care home groups we looked at had cost-control KPIs. However, this cost-focused approach has its limits, including “what can be achieved in terms of efficiency savings without impacting on the quality of service” (Anchor Trust, 2018, p. 5). As these limits are reached, many care groups have turned to increasing the proportion of self-funded residents in their homes, as this helps to “create [financial] stability across the whole estate” (The Orders of St John Care Trust, 2020, p. 16). We will examine the issue of cost-control in care homes in more detail in the discussion section below.
6 Discussion and recommendations
Throughout this report, we have looked to answer the question: what happens to working conditions and quality of care when investment firms take over UK care homes? We interviewed sixteen care workers, fourteen of whom were working in the care home at the time it changed hands. The interviews confirmed a highly challenging environment across the sector, regardless of ownership type. Notably, however, despite not mentioning that we were interested in investment firm ownership in our recruitment materials, twelve out of sixteen eligible participants who approached us were working in homes taken over by investment firms (compared to two participants working in a charity owned care home, one in a small private business owned home, and one in a home owned by a large public company).
We developed five core themes from analysing our interviews with these care workers, as presented in Section 4. The first theme detailed the various ways that interviewees’ employers exploited them, from reducing staff benefits to chronically understaffing the care homes (Section 4.1). It also highlighted the crucial role of staff in protecting residents from the negative impacts of this understaffing. The second theme built on these insights, going into the range and depth of under-resourcing in the sector, beyond staff shortages (Section 4.2). From rationing medical and sanitary supplies and food, to neglecting care home maintenance and failing to deliver enriching activities for residents, interviewees painted a picture of a care sector that has been stripped back to the bare bones.
Our third theme reflected participants’ views that their employer was often mismanaging their care home, and that, in some instances, they were trying to conceal the problems caused by that mismanagement from the industry regulator (Section 4.3). This perceived mismanagement was compounded by the findings from our fourth theme: a failure of internal communications, with ineffective channels for feedback and a lack of transparency from the company, leaving participants feeling ignored and frustrated (Section 4.4). Finally, in the fifth theme, we heard from interviewees that they felt their employer was primarily involved in the care sector to make money, and that they didn’t care about the wellbeing of staff or residents (Section 4.5). This theme tied together the experiences across the four other themes, offering a glimpse into the perceived motivations behind the chronic understaffing and under-resourcing uncovered.
We complemented the thematic analysis with a review of key business metrics and performance indicators from the accounts of fifteen of the largest care home groups in the UK. We found that in 2020 the average remuneration ratio of the highest paid director to the average employee was substantially higher in for-profit groups (38:1 in investment firm-owned groups; 63:1 in groups not owned by investment firms) compared to not-for-profits (29:1). When looking at KPIs we found a greater focus on cost-control among not-for-profit groups. This may be explained in part by the higher proportion of residential care homes within these care groups and the smaller average number of beds per care home, both of which limit providers’ ability to manage the trend towards increasingly complex and costly residents in this part of the market. Additionally, the vast majority of care home groups of all ownership types had KPIs focused on occupancy and income, with fewer than half including indicators of care quality or staff wellbeing (this was particularly pronounced in investment-firm-owned groups).
In all, our empirical findings confirm much of what has been written about before in the literature, including low staffing levels, restrictions to budgets that affect food, maintenance, equipment and medical supplies, and worse quality care as a result of these factors (Burns, Hyde and Killett, 2016; Bos and Harrington, 2017; Horton, 2019). See Section 2 again for a full discussion of these issues.
Building on this, we elaborate several novel findings below: first, cost minimisation targets are present across large care home groups, regardless of ownership type, but our thematic analysis suggests they may be having a more negative impact in those homes where profit is a primary consideration (Section 6.1); second, attempts by large companies to counter the communication and control problems associated with complex corporate structures are negatively impacting staff morale and quality of care (Section 6.2); and third, charities may also be part of large company groups that display similar structures to for-profit care groups, and may therefore be susceptible to some similar dynamics (Section 6.3).
6.1 The impacts of cost minimisation
First, our thematic analysis indicated a clear difference in the way that participants from investment-firm-owned care homes spoke about understaffing and budget restrictions as compared to those participants working in family-run care homes or those owned by small businesses (see Sections 4.1 and 4.2). The latter emphasised the hap-hazard or ‘wheeler dealer’ nature of their owners’ engagement with the care home, where the former tended to speak more about fixed and deliberate policies aimed at reducing staffing levels, delaying maintenance requests, and restricting access to medical or housekeeping supplies, among other things.
However, when looking at the financial accounts of the largest UK care home chains, we found that cost minimisation targets (of the sort likely to impact staffing and care expenditures) were present in the accounts of 8/15 of the care home chains examined, across all ownership types (see Section 5). Our findings of care worker exploitation and sub-par service delivery (see Sections 4.1 and 4.2) may therefore, at least in part, be driven by other factors than owner type. For example, larger care home size, and being part of a care home chain, have both been found to be associated with worse quality care in a variety of contexts (Anderson et al., 2003; You et al., 2016; Baldwin et al., 2017), and investment-firm-owned groups are amongst the largest operators in the care home market. Chain size may therefore also be driving the quality issues we picked up, in addition to owner type.
Nonetheless, investment-firm-owned care homes are cost-minimising in a context where they are also attempting to deliver something in the region of a 12% return on investment to their investors (Laing, 2008). In a revenue restricted environment (like the one created by austere welfare policies), this is likely to lead to a downward pressure on wages, staff benefits, investments in care home improvement, and quality of care, as companies only have a limited number of ways that they can navigate cost pressures (Schmitt, 2013). This might go some way to explaining why the vast majority of eligible participants who approached us to participate in the study were from investment-firm-owned care homes, despite the cost-minimisation KPIs being present across ownership types. Most importantly, our thematic analysis indicates that cost minimisation strategies focused on reducing staff time and rationing medical and food supplies, no matter who is implementing them, leads to poor outcomes for residents and care workers.
6.2 Communication and control in large chains
One issue that emerged in Sections 4.3 and 4.4 was problems with communication and control in large care home chains. For example, many of our participants spoke about a lack of opportunities to communicate with their employer, which led them to feel isolated, disempowered and unable to effect change in their workplace. Additionally, several participants said that they felt their employer was often prioritising paperwork over care. In combination, these themes could be interpreted in a couple of different ways. Through one lens, ineffective or absent channels for communication might reflect a lack of interest in staff wellbeing and/ or respect for staff knowledge about how best to deliver care to residents. It could even be part of a deliberate attempt to disempower staff, with the focus on paperwork reflecting a desire to cover up poor service quality. This fits with our participant Sarah’s experience of being told to lie on paperwork, and of being removed from shift when the CQC came to inspect her care home. It also aligns with findings from previous research studies, such as Burns et al. (2016) and Horton (2017), which suggest that strategies that shift the costs of austerity and financialisation onto staff and service users are being use in investment-firm-owned care homes.
Alternatively, we could interpret these themes through a more technocratic lens. In their latest report, industry analyst LaingBuisson talks about how large care home operators experience “portfolio control and communication issues” (LaingBuisson, 2021, p. 15). Larger chains may therefore be relying on enhanced monitoring and reporting processes to manage challenges. For example, Akari Care (a large care home company owned by American private equity firm, The Carlyle Group) talked about how the roll out of a new electronic care planning system will: “assist in maintaining and improving future regulatory compliance” (Akari Care Limited, 2020, p. 4). Regardless of the motivation, our interview data suggest that the onerous administration and paperwork requirements placed on staff are not being properly resourced and many staff feel that they are taking valuable time away from caring duties. Further, these strategies appear not to be effectively addressing the issues with control and communication either, at least from the staff’s perspective, as they are still reporting an inability to communicate with the company and to affect change in the home.
6.3 Does ownership type really matter?
We found that those participants who worked in charity-owned care homes were raising some of the same issues as those found in investment-firm-owned homes; in particular, around a lack of transparency from their employer, as well as onerous paperwork taking time away from care. These participants did not, however, appear to feel that there was a tangible impact of these issues on the quality of care being delivered to residents. This is in quite stark contrast to most other interviewees (who felt that under-resourcing and expanded workloads were directly impacting care) and might indicate something about the severity of the under-resourcing in the investment-firm-owned homes we sampled, as compared to the charity-owned ones. These findings resonate with the broader literature, which generally finds that not-for-profit care homes deliver, on average, higher quality care, both in the UK and other countries (Comondore et al., 2009; Barron and West, 2017).
Nonetheless, both of our charity-sector participants pointed out that, even within the not-for-profit portion of the care market, there are corporate structures and financial tactics at play, including high salaries for directors, the splitting of the property and operating companies, related offshore entities, and tax minimisation strategies. Our analysis of director remuneration in the largest UK care home groups indeed found that not-for-profit care home chains had large pay disparities, with the highest paid directors being paid on average 29 times the pay of the average employee (although this was not as high as the ratio in for-profit care homes, which was at least 38:1). Also within our sample we can see the marks of other complex corporate structures. For example, Sanctuary Housing Association has an internal prop-co, op-co split and, according to their 2020 accounts, has one subsidiary company registered in the Isle of Man (Sanctuary Group, 2020). Although the extent of complexity within the company structures, the size of pay disparities, and the degree of any financial extraction is clearly not on the same scale as the for-profit care chains (Corlet Walker, Druckman and Jackson, 2021), these observations highlight the depth and breadth of issues in the care sector and indicate a need for thoughtful transformation across the board.
6.4 Recommendations: what next for the UK’s adult social care sector?
Finally, we consider what our findings might mean for practitioners and policymakers, moving forwards. In particular, we reflect directly on what participants felt good ownership would look like for them, as well as offering recommendations based on our synthesis of the findings from both the thematic analysis and the review of company accounts.
Remove profit from the care sector
A number of participants suggested that moving to not-for-profit models of care delivery (either a national care service or a mix of not-for-profit provider types) would deliver benefits such as more transparency and accountability, improved accessibility, and greater investment directly in staff and care. Their views on this are supported by the literature which finds quality of care and wages to be higher in not-for-profit care homes. There are also likely to be fewer complex corporate structures and less movement of public money to offshore companies within not-for-profit groups. In addition to these benefits, our analysis suggests that the care sector is under enormous cost pressures from all sides, and that removing profit from the mix (in combination with increasing government funding into the sector) might relieve one of those pressures, particularly for care homes in chains that are currently heavily financialised.
Reduce the size of company groups
Reducing the size and complexity of company groups might help to address the challenges of distant ownership and onerous paperwork. It is clear that large corporate group structures do not mesh well with participants’ ideas of what is needed to effectively run a care home in a flexible and person-centred way. They felt that their employers were unresponsive to feedback, and many felt that the focus on paperwork was taking time away from caring duties. This idea of disjointedness between the corporate structures of the care group as a whole and the reality of day-to-day care was expressed by a number of participants. Further, problems with control and communication have been reported by industry analysts too, as well as in the company accounts of larger providers. Reducing the size of care groups would likely enable a greater responsiveness to the needs of individual care homes, particularly if combined with actions to relieve cost pressures (i.e., sufficient funding from local authorities and the removal of excessive rent-seeking by investors) and to empower staff to feed into decision-making processes (see more below). This may also support care quality improvements, as smaller care home chains tend to be associated with better quality.
Support and empower staff
Many participants highlighted the need for companies to invest in their staff teams, in terms of training, adequate recognition, and pay commensurate with the difficultly of the job, not only to support staff in feeling valued, but also to attract and retain high quality staff. Participants also felt that more staff were needed, not only in caring roles, but also in housekeeping, administration, etc, and that adequate resourcing should be provided when care staff are asked to take on additional responsibilities, such as extra paperwork. Given how crucial staff are to quality of care, investing in staff is likely to have substantial knock-on benefits for residents.
Beyond adequate staffing levels and proper pay and recognition, participants also emphasised the benefits that could be reaped by listening to staff and involving them in the decision-making processes. There are a number of ways that staff could be empowered within their workplace, from improving formal feedback channels, to union membership, and even co-operative ownership models. Each of these options would support staff to be better able to communicate and positively impact the needs of residents, as well as their own needs. They would also reflect their position (alongside service users) as the most knowledgeable stakeholders when it comes to determining how to deliver high quality care in their particular home.
Improve data availability
Based upon participants’ responses and our review of the largest care groups, there seems to be both an excessive burden of regulatory paperwork and yet a lack of useful care quality information available. This is something that has also recently been raised by a group of academics who have called for a “minimum data set for older adult care homes in the UK”, and who are undertaking trials to establish the most effective structure for that data (Burton et al., 2022). Richer care quality and staffing datasets in the US—e.g., Nursing Home Compare website—have facilitated extensive and insightful analysis. Replicating and building on this in the UK would improve our understanding of the drivers of quality care and the state of working conditions in the sector. To achieve these improvements, greater resourcing for the CQC and other data collection bodies will be key.
6.5 Conclusions
Unpicking the story of how ownership type impacts quality of care and working conditions is complex and challenging, in part because of the opaque nature of the care homes industry. The financial structures and management strategies of investment firms are often not directly observable, and outcomes data on quality of care and working conditions for the UK are sparse. Through analysing a series of interviews with care workers and reviewing the accounts of the largest UK care home companies, we have shed light on the question of what happens when investment firms take over care homes, and how this impacts quality of care and working conditions. Our findings align with the growing consensus from the literature that investment firms employ strategies to reduce staffing levels and minimise care costs, and that this has substantial, negative impacts on quality of care and working conditions.
Beyond a focus on cost minimisation and financial extraction, we have also elaborated other pathways through which the experiences of residents and workers might be negatively impacted by investment firm owners. These include: the exploitation of care workers through the creation of a hostile work environment (in which staff are made to feel replaceable) and a reliance on their commitment and sense of responsibility to residents; the simultaneous lack of open feedback channels for staff alongside the implementation of onerous monitoring and paperwork processes, leaving staff feeling disempowered and frustrated; and the lack of transparency and accountability within the care home company, creating an atmosphere of mistrust and uncertainty about the future.
These findings point towards three core conclusions. One, that a transition towards a non-profit care sector could help to limit the financial leakage out of the sector and relieve tensions between investors, workers and service users. Two, that reducing the size and complexity of care home groups could offer a fruitful avenue for mitigating problems with communication and transparency. And three, that empowering care workers to have a say in how their workplace is run would likely improve working conditions and quality of care within the sector.
References
Age UK (2019) ‘Estimating need in older people: Findings for England’. London, UK: Age UK, pp. 1–23.
Akari Care Limited (2020) ‘Annual Report and Financial Statements for the year ended 31 October 2020’. Leeds, UK: Companies House, pp. 1–25.
Anchor Trust (2018) ‘Annual Report & Financial Statements For the year ending 31 March 2018’. London, UK: Companies House, pp. 1–83.
Anderson, R. I. et al. (2003) ‘Nursing home quality, chain affiliation, profit status and performance’, Journal of Real Estate Research, 25(1), pp. 43–60. doi: 10.1080/10835547.2003.12091100.
Ayash, B. and Rastad, M. (2021) ‘Leveraged buyouts and financial distress’, Finance Research Letters, 38(October 2019), p. 101452. doi: 10.1016/j.frl.2020.101452.
Baldwin, R. et al. (2017) ‘Does size matter in aged care facilities? A literature review of the relationship between the number of facility beds and quality’, Health Care Management Review, 42(4), pp. 315–327. doi: 10.1097/HMR.0000000000000116.
Barron, D. N. and West, E. (2017) ‘The quasi-market for adult residential care in the UK: Do for-profit, not-for-profit or public sector residential care and nursing homes provide better quality care?’, Social Science and Medicine, 179, pp. 137–146. doi: 10.1016/j.socscimed.2017.02.037.
Blakeley, G. and Quilter-Pinner, H. (2019) ‘Who Cares? The Financialisation of Adult Social Care’. London, UK: Institute for Public Policy Research, pp. 1–12. Available at: www.ippr.org/research/publications/financialisation-in-social-care.
Bos, A. and Harrington, C. (2017) ‘What happens to a nursing home chain when private equity takes over? A longitudinal case study’, Inquiry: The Journal of Health Care Organization, Provision, and Financing, 54, pp. 1–10. doi: 10.1177/0046958017742761.
Braun, V. and Clarke, V. (2006) ‘Using thematic analysis in psychology’, Qualitative Research in Psychology, 3(2), pp. 77–101. doi: 10.1191/1478088706qp063oa.
Bunting, M. (2020) Labours of Love: The Crisis of Care. London, UK: Granta Books.
Burns, D. et al. (2016) ‘WHERE DOES THE MONEY GO? Financialised chains and the crisis in residential care Diane’, Centre for Research on Socio-Cultural Change, (March), pp. 1–68. Available at: http://www.cresc.ac.uk/medialibrary/research/WDTMG FINAL -01-3-2016.pdf.
Burns, D. J., Hyde, P. J. and Killett, A. M. (2016) ‘How financial cutbacks affect the quality of jobs and care for the elderly’, Industrial and Labor Relations Review, 69(4), pp. 991–1016. doi: 10.1177/0019793916640491.
Burton, J. K. et al. (2022) ‘Developing a minimum data set for older adult care homes in the UK: exploring the concept and defining early core principles’, The Lancet Healthy Longevity, 3(3), pp. e186–e193. doi: 10.1016/S2666-7568(22)00010-1.
Cabinet Office (2021) Cabinet Office senior officials ‘high earners’ salaries, GOV.UK. Available at: https://www.gov.uk/government/publications/senior-officials-high-earners-salaries.
CMA (2017) ‘Care homes market study: Financial analysis working paper’. London, UK: Competition and Markets Authority, pp. 1–48.
Comondore, V. R. et al. (2009) ‘Quality of care in for-profit and not-for-profit nursing homes: Systematic review and meta-analysis’, BMJ (Online), 339(7717), pp. 381–384. doi: 10.1136/bmj.b2732.
Corlet Walker, C., Druckman, A. and Jackson, T. (2021) ‘Careless finance: Operational and economic fragility in adult social care’. Guildford: Centre for the Understanding of Sustainable Prosperity, pp. 1–42. Available at: cusp.ac.uk/careless-finance.
Corlet Walker, C., Druckman, A. and Jackson, T. (2022) ‘A critique of the marketisation of long-term residential and nursing home care’, The Lancet Healthy Longevity, 3(4), pp. 1–9.
CQC (2022) Dataset: CQC care directory (01 March 2022), Care Quality Comimssion. Available at: https://www.cqc.org.uk/about-us/transparency/using-cqc-data.
Dowling, E. (2021) The Care Crisis: What Caused It and How Can We End It? London, UK: Verso.
Fenton, W. et al. (2021) ‘The state of the adult social care sector and workforce in England’, Skills for Care, pp. 1–141. Available at: www.skillsforcare.org.uk.
Forrester-jones, R. and Hammond, M. (2020) ‘Adult Social Care and Unmet Needs’. Access Social Care, pp. 1–49.
Gupta, Atul et al. (2021) ‘Does Private Equity Investment in Healthcare Benefit Patients ? Evidence from Nursing Homes’, NBER WORKING PAPER SERIES. Cambridge, MA, pp. 1–76.
Harrington, C. et al. (2001) ‘Does investor-ownership of nursing homes compromise the quality of care?’, International Journal of Health Services, 32(2), pp. 315–325. doi: 10.2190/EBCN-WECV-C0NT-676R.
Harrington, C. et al. (2012) ‘Nurse staffing and deficiencies in the largest for-profit nursing home chains and chains owned by private equity companies’, Health Services Research, 47(1 PART 1), pp. 106–128. doi: 10.1111/j.1475-6773.2011.01311.x.
Horton, A. (2019) ‘Financialization and non-disposable women: Real estate, debt and labour in UK care homes’, Environment and Planning A, 0(0), pp. 1–16. doi: 10.1177/0308518X19862580.
Horton, A. E. (2017) Financialisation of Care: Investment and organising in the UK and US. Queen Mary, University of London.
Huang, S. S. and Bowblis, J. R. (2019) ‘Private equity ownership and nursing home quality: an instrumental variables approach’, International Journal of Health Economics and Management, 19(3–4), pp. 273–299. doi: 10.1007/s10754-018-9254-z.
Kay, R. and Hildyard, L. (2020) ‘Pay ratios and the FTSE 350: an analysis of the first disclosures’, (December). Available at: https://highpaycentre.org/pay-ratios-and-the-ftse-350-an-analysis-of-the-first-disclosures/.
Knight Frank (2021) ‘2021 UK Care Homes Trading Performance Review’. London, UK: Knight Frank, pp. 1–14. Available at: https://content.knightfrank.com/research/548/documents/en/care-homes-trading-performance-review-2020-7621.pdf.
Kotecha, V. (2019) ‘Plugging the leaks in the UK care home industry. Strategies for resolving the financial crisis in the residential and nursing home sector’. London, UK: Centre for Health and the Public Interest, pp. 1–53.
Laing Buisson (2018) ‘Care Markets Annual Survey of UK Local Authority Usual Costs’, (July 2017), pp. 1–18. Available at: https://www.laingbuisson.com/wp-content/uploads/sites/3/2017/07/CareMarkets_UsualCosts_20172018.pdf.
Laing, W. (2008) ‘Calculating a fair market price for care: A toolkit for residential and nursing homes’. Bristol, UK: The Policy Press, pp. 1–56.
LaingBuisson (2018) Care Homes for Older People – UK Market Report. 29th edn. London, UK: LaingBuisson.
LaingBuisson (2021) Care Homes for Older People UK Market Report. 31st edn. London, UK: LaingBuisson.
NHS Digital (2022) ‘NHS Staff Earnings Estimates, December 2021, Provisional Statistics – NHS Digital’, (December 2021). Available at: https://digital.nhs.uk/data-and-information/publications/statistical/nhs-staff-earnings-estimates/december-2021-provisional-statistic.
Pradhan, R. et al. (2014) ‘Private equity ownership of nursing homes: Implications for quality’, Journal of Health Care Finance, 42(2), pp. 1–14.
Sanctuary Group (2020) ‘Annual Report and Financial Statements 2019/2020’, pp. 1–176.
Schmitt, J. (2013) ‘Why Does the Minimum Wage Have No Discernible Effect on Employment?’, Center for Economic and Policy Research, (February), pp. 1–28.
Stevenson, D. G. and Grabowski, D. C. (2008) ‘Private equity investment and nursing home care: Is it a big deal?’, Health Affairs, 27(5), pp. 1399–1408. doi: 10.1377/hlthaff.27.5.1399.
Tamara Konetzka, R., Yan, K. and Werner, R. M. (2021) ‘Two Decades of Nursing Home Compare: What Have We Learned?’, Medical Care Research and Review, 78(4), pp. 295–310. doi: 10.1177/1077558720931652.
The Orders of St John Care Trust (2018) ‘Annual Report & Accounts for the year ended 31 March 2018’. Witney, UK: Companies House, pp. 1–67. Available at: http://www.osjct.co.uk/.
The Orders of St John Care Trust (2020) ‘Annual Report & Accounts for the 12 months ended 31 March 2020’. Witney, UK: Companies House, pp. 1–84. Available at: http://www.osjct.co.uk/.
UNISON (2021) ‘Care employers still not giving sick pay to Covid-hit staff, says UNISON survey’. London, UK: UNISON. Available at: https://www.unison.org.uk/news/press-release/2021/06/care-employers-still-not-giving-sick-pay-to-covid-hit-staff-says-unison-survey.
You, K. et al. (2016) ‘Do nursing home chain size and proprietary status affect experiences with care?’, Med Care, 5(3), pp. 229–234. doi: 10.1097/MLR.0000000000000479.Do.
Notes
[1] This includes companies who have a significant partnership with an investment firm. We class private equity, hedge funds, real estate investment trusts, pension funds, and private companies that invest for a wide range of investors as investment firms.
[2] Turnover includes income from all company activities, including those not directly related to the provision of adult social care.
[3] This is EBITDAR profitability as a % of turnover. EBITDAR stands for earnings before interest, taxes, depreciation, amortization, and rent. It is a common industry measure of operating profitability. For Four Seasons, Sanctuary, Minster Care Group, Orders of St John Care Trust, and Priory Group did not offer figures for rental expenditure, and so their figures are for EBITDA, which is EBITDAR with rent expense added in. All figures exclude exceptional items.
[4] As a % of turnover. For Four Seasons this is profits from continuing operations only. For Orders of St John Care Trust it is net income for the year, before other recognised gains and losses.
[5] This is average number of employees, except for Sanctuary Housing Association where it was Full Time Equivalents (FTE).
[6] Since its 2020 year-end, the company has been acquired by funds managed by Stirling Square Capital Partners, a private equity firm.
[7] There are an estimated 105,000 vacancies in the adult social care sector (Fenton et al., 2021)
[8] EBITDAR is is a common industry measure of operating profitability. For Four Seasons, Sanctuary, Minster Care Group, Orders of St John Care Trust, and Priory Group we were unable to find figures for rental expenditure and so excluded them from the average. All figures exclude exceptional items.
[9] Remuneration for employees consists of the following employee costs: wages and salaries, social security costs, and pension costs. Remuneration for directors consists of director costs such as: emoluments and company contributions to pension schemes.
[10] Four groups were not included in this calculation because we couldn’t calculate enough remuneration values to carry out a like for like comparison over time, these were: one for-profit investment-firm-owned group (Four Seasons), two for-profit groups not owned by investment firms (Caring Homes; Priory Group), and one not-for-profit group (Sanctuary).
[11] Remuneration per employee excludes directors remuneration. It is calculated as employees’ remuneration, divided by the number of employees.
[12] Remuneration per director excludes company directors whose remuneration was paid for by other group companies. It is calculated as directors’ remuneration, divided by the number of directors.
Download
Please cite document as: Corlet Walker C, Kotecha V, Druckman A and T Jackson 2022. Held to ransom: What happens when investment firms take over UK care homes. CUSP Working Paper Series, No 35. Guildford: Centre for the Understanding of Sustainable Prosperity. The full paper is available for download in pdf (2.5MB).
Acknowledgements
We would like to thank the sixteen participants who enabled this project to take place. Thanks to Gavin Edwards from UNISON for his support throughout the process of this research project, to Linda Gessner for her feedback on earlier drafts, and to Anastasia Loukianov and Keith Walker for many fruitful discussions about thematic analysis. This work was supported by the Economic and Social Research Council (ESRC; grant number ES/P00072/X). It also forms part of the ESRC-funded interdisciplinary research programme at the Centre for the Understanding of Sustainable Prosperity (grant number ES/M010163/1). We also gratefully acknowledge the support of UNISON in part-funding this work.